Is A Biological Heart Valve or Mechanical Heart Valve Right For You?
When a heart valve is severely damaged and cannot be reliably repaired our best option is its replacement with a valve prosthesis or a mechanical heart valve. Let’s talk about these “spare parts” available to us for the treatment of heart valve disease.
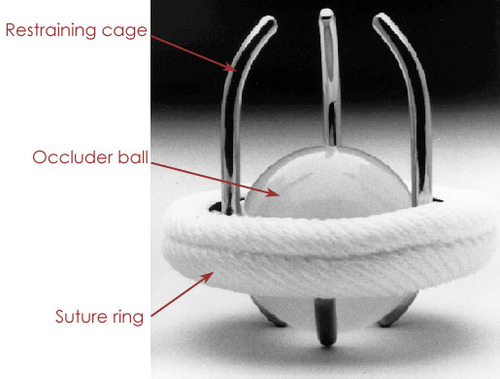 The first artificial heart valve to get widespread acceptance and clinical use among cardiac surgeons was the so called “ball-and-cage” valve. It consists of a silicon ball that opens and closes the valve opening by moving up and down within a metal cage. The actual design of this valve was inspired by an older invention, patented in 1858 and marketed in the US to be used as a wine bottle stopper!!
The first artificial heart valve to get widespread acceptance and clinical use among cardiac surgeons was the so called “ball-and-cage” valve. It consists of a silicon ball that opens and closes the valve opening by moving up and down within a metal cage. The actual design of this valve was inspired by an older invention, patented in 1858 and marketed in the US to be used as a wine bottle stopper!!
The technical evolution and research commitment to create the perfect heart valve substitute has been carrying on for the last 45 years. The design and engineering behind contemporary valves is directed to improved reliable and durable performance.
Today we can pick a variety of heart valve prostheses from our surgical supply shelves. They come in different sizes and designs to fit the individual patients’ needs. The choice of a valve substitute is in fact tailored to the patient. It takes into account multiple factors, such as age, sex, personal preferences, level of expected physical activity, plans to get pregnant, etc. We can essentially divide the valve prostheses in two broad categories, each with its own pros and cons: mechanical valves and biological valves.
Mechanical Heart Valves
Mechanical Heart Valves can be simply described as a steel alloy ring with an outer cloth suture ring and two half moon shaped leaflets hinged inside it.
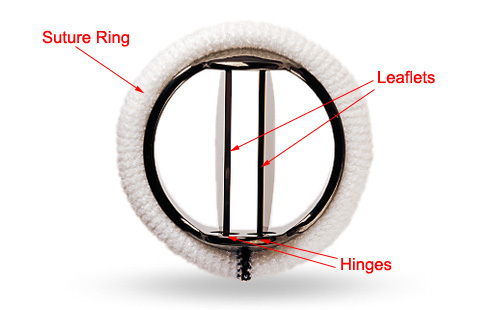
The leaflets open and close pretty much like window shutters. All the mechanical heart valve components are coated with pyrolytic carbon. This compound decreases the chance of blood clotting on the valve surface, it is very hard, it does not wear out and guarantees a virtually unlimited duration of the valve in ideal conditions.
The main disadvantage is that patients who received a mechanical valve will have to take blood thinners for the rest of their lives to prevent the formation of dangerous blood clots. This is a necessary and important therapy because normal blood tends to form clots when it is in contact with an artificial surface.
Blood clots can in fact jam the mechanical valve in an open or closed position causing stenosis, insufficiency or a combination of both. Some clots can come loose and cause a stroke or a heart attack by traveling from the prosthetic valve to the arteries that supply the heart (coronary arteries) or the brain (carotid arteries). In order to prevent these complications, the effect of the blood thinners is monitored by blood tests to make sure that the appropriate level of blood thinning is maintained within its best therapeutic range.
If the level is too low the blood might clot on the valve. On the other hand, if the level is too high there is a higher risk of spontaneous bleeding. Patients’ education and compliance is very important and can certainly improve the management of coumadin therapy.
Biological Heart Valves
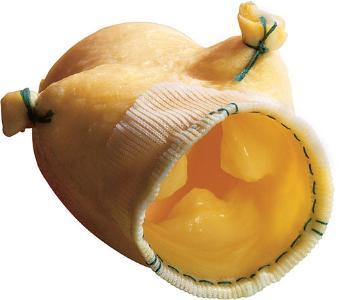
Biological Heart Valves are made of tissues and valves derived from animals or human donors. Their biggest advantage is that they do not cause blood clotting on their surface and truly replicate the form and function of the normal human valve. The biological heart valve you see in the following picture is a pig valve mounted on a frame and suture ring to facilitate its implant in our heart patients.
There is a widespread misconception out there that these valves could be “rejected” by the body as if they were a sort of transplant. This is simply not true. These biological cow, pig, equine or human valves are all treated with chemical agents that erase any surface antigens capable of stimulating an immune response to them and improve their durability and resistance to calcification over time.
The following is one of the bench studies I participated in to demonstrate the use of chemical treatments to improve the durability of biological tissues in cardiac surgery:
Liao K., Frater R.W.M., LaPietra A., Ciuffo G., Ilardi C.F., Seifter E. Time-Dependent Effect of Glutaraldehyde on the Tendency to Calcify of Both Autografts and Xenografts. Annals of Thoracic Surgery 1995 Aug.; 60 (2 suppl.): S343-7

Another recent version of pig valve prosthesis is also available in our operating rooms. It is prepared without an actual mounting frame. The difference here is that a portion of the pig aorta is harvested and preserved along with the valve attached to it. This type of valve prosthesis can be used to implant a valve with a larger diameter or to replace that portion of the aorta known as the Aortic Root when needed. The following is a picture of this new type of valve:
 The important thing to remember about biological valves is that they function exactly like human valves and do not need life long coumadin therapy because they do not tend to form blood clots on their natural biologic surface.
The important thing to remember about biological valves is that they function exactly like human valves and do not need life long coumadin therapy because they do not tend to form blood clots on their natural biologic surface.
Unlike the mechanical valves, though, their duration is not unlimited. With time they tend to wear out and stiffen and compromise their function. In patients with a long life expectancy they might even need to be replaced with a second valve. The latest biological valves are treated with special chemicals that delay the calcification and stiffening process.
These treatments give improved durability, especially in older patients. As you can imagine the goal of all research efforts in this field is to create the perfect valve, with unlimited duration and virtually no clotting complications.
Now that we know what these valves are about we can make an intelligent choice!
Chances are that even after this brief description you would still like to ask me the classic and time honored question: “Which valve would you use for yourself or for your mother? Well, here is some more insight in our clinical experience that can guide your choices. Every patient has a special situation and preferences that can tip the balance one way or the other. It is very important to have an in-depth discussion with your heart specialist about it. Don’t be shy about asking questions and voicing your concerns. We include in our considerations age, life style expectations, the prospect of future pregnancies, other medical conditions.
- Biological valves calcify and deteriorate faster in younger patients. If you have a younger patient who needs a valve replacement you might be concerned about having to re-replace the valve more than once in his or her life time. Most patients do not enjoy the prospect of multiple open heart operations. In this case, many heart surgeons could be more inclined to recommend the use of a mechanical valve. On the other hand, coumadin therapy can affect a pregnancy and cause damage to the fetus.
A young lady who is planning to have a family might therefore prefer to have a biological valve that does not require blood thinners and does not jeopardize her pregnancies. She’ll have her children and, if necessary, she’ll have a redo valve replacement later on in life. You could also be confronted with a young man that enjoys football, rock climbing and traveling to every God forsaken corner of the world. He prefers a biological valve and no coumadin to make sure he does not risk serious bleeding when he plays rough and does not need to find a lab to test his blood thinner while he is traveling away from home.
- A mechanical valve and coumadin for the rest of your life comes with a price. There are two main problems related to this situation:
1. The blood thinning therapy needs to be religiously kept up and monitored with frequent blood tests to avoid the blood clotting on the mechanical valve itself. Blod clots can jam the valve open or close and/or can come loose in the circulation causing strokes, heart attacks, kidney failure, intestinal gangrene, and other embolic complications. On the other hand, thinned out blood means more chances of serious bleeding complications.
2. Our statistical studies show that life long coumadin therapy with a mechanical valve carries an overall 2% per year major complication rate. If you do the math (2% times the number of years you expect to live) you can see that if you have a whole life to look forward to, you might also have a very high chance to experience a major complication. At this point the 2 to 3% risk of an elective valve re-replacement fifteen years after the first operation sounds much safer than a mechanical valve and coumadin therapy for the rest of your life. Keep also in mind that not all mechanical valves last forever. Mechanical failures are extremely rare but some of them (10 to 15%) might still need to be re-replaced because of infections, jamming, clots.
- What would I want for myself? By now you probably guessed. I am in my early fifties, I have a physically demanding job, I enjoy traveling and sport activities. I don’t want any changes or limitations to my life style. The prospect of coumadin therapy for the next few decades and the higher risk of a stroke or a cerebral hemorrhage scares me a lot more than the prospect of a redo operation 10 to 15 years later in the hands of an expert surgeon. I would definitely choose a biological valve for myself and seek a minimally invasive approach.
In summary, there are many factors that can influence your choice. It is important for you to know your options and then take the time to calmly discuss them with an expert physician to choose what you think is best for you.
Schedule A Consultation With Expert Heart Surgeon, Dr. Ciuffo
If you are interested in receiving a minimally invasive surgery for your aortic valve replacement or repair, give our expert heart surgeon, Dr. Ciuffo, a call at (712) 294-7055 or contact us online.
