by targetmarket | Jan 31, 2024 | Heart Health
Your heart rate is an integral part of how your body functions, but can also be a way to tell if you are overexerting your body or not. Your heart rate or pulse has a standing level (the rate during normal activity) and a peak heart rate (when exercising full force.) Your suggested target heart rate (THR) is going to be about 64-76% of your peak level. For those who want to exercise but are not sure of the right exercise regimen, we suggest seeking medical advice. Here at Minimally Invasive and Bloodless Heart Surgery with Dr. Ciuffo, we are going to dive into what you need to know about your target heart rate. Understanding Your Target Heart Rate Understanding your target heart rate is especially important for anyone engaging in cardiovascular exercise or striving to improve their overall fitness. Your target heart rate is a range that indicates the optimal intensity at which your heart should be working during exercise to achieve maximum benefits. It serves as a valuable guide, helping you tailor your workouts to suit your fitness goals, whether you’re aiming for weight loss, improved cardiovascular health, or enhanced endurance. Tracking Your Target Heart Rate Monitoring your heart rate during exercise can be done manually by checking your pulse at your wrist or neck or, more conveniently, with a heart rate monitor. Many fitness trackers and smartwatches come equipped with heart rate monitoring features, making it easy to keep track of your intensity levels in real-time. Aerobic Versus Anaerobic Training Aerobic and anaerobic training are two distinct types of exercise that target different energy systems... 
by targetmarket | Nov 30, 2023 | Heart Health
The intricate connection between mental health and physical well-being has been a subject of growing interest in recent years. While it’s well-known that mental health issues like anxiety and depression can profoundly impact one’s quality of life, what’s often overlooked is their potential to affect physical health, particularly the heart. Mental Health And Heart Health The complex relationship between mental health and heart health highlights the ways in which our emotional well-being can significantly influence the cardiovascular system. Dr. Ciuffo’s practice emphasizes the integration of medical and psychological care to provide the best possible outcomes for his patients through a wide range of advanced options and procedures in modern heart surgery. Stress Stress is an everyday part of modern life, and while some stress is normal and even beneficial, chronic stress can wreak havoc on both mental and physical health. When you experience stress, your body releases hormones like cortisol and adrenaline, which prepare you for a “fight or flight” response. However, prolonged exposure to stress can lead to persistently high levels of these hormones, contributing to increased heart rate, elevated blood pressure, and inflammation, all of which raise the risk of heart disease. Depression Depression is a mood disorder that affects millions of people worldwide. Research has shown that individuals with depression are more likely to develop heart disease. The exact mechanisms behind this link are complex, but it’s believed that the combination of lifestyle factors associated with depression (such as poor diet, lack of exercise, and smoking) and the physiological effects of depression on the body (including inflammation and blood clotting) can contribute to heart problems. Anxiety... 
by targetmarket | Nov 15, 2023 | Heart Health
Cardiovascular disease remains the leading cause of death worldwide, and it poses a significant threat to men’s health. While cardiovascular risk affects both genders, men often face unique challenges and factors that increase their susceptibility. Understanding these risk factors and taking proactive steps toward heart health is crucial for men of all ages. Cardiovascular Risk In Men With heart disease being the leading cause of death for men in the United States, accounting for 1 in 4 male deaths, it is essential to explore the key aspects of cardiovascular risk that men need to be aware of. Dr. Ciuffo is an expert in high-risk heart surgery cases. His techniques and protocols allow for excellent results and greatly improved quality of life. Continue reading to learn more about cardiovascular risk in men, and what you need to know. Age and Heart Health Age plays a critical role in cardiovascular risk. As men grow older, their risk of heart disease tends to increase. According to the American Heart Association, men over the age of 45 are at greater risk of heart disease, especially if they have a family history of heart conditions. However, this doesn’t mean that younger men are immune to heart problems. Lifestyle choices and genetic factors can influence heart health at any age. Hypertension Hypertension, or high blood pressure, is often referred to as the “silent killer” because it typically shows no symptoms until it leads to more severe health issues. Men are more likely than women to develop hypertension, especially as they age. High blood pressure puts extra strain on the heart and blood vessels, increasing the... 
by targetmarket | Oct 31, 2023 | Heart Health
Your heart is the engine that powers your body, which means making heart healthy choices should be a top priority. Heart disease remains one of the leading causes of death worldwide, but the good news is that many of the risk factors are controllable. Heart Healthy Tips Here at Minimally Invasive and Bloodless Heart Surgery with Dr. Ciuffo, we will explore some By making simple lifestyle changes and adopting heart healthy habits, you can significantly reduce your risk of heart disease and enjoy a longer, healthier life. tips to keep your heart in optimal condition. 1. Eat a Balanced Diet A heart healthy diet is the foundation of cardiovascular health. Focus on consuming a variety of nutrient-rich foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit your intake of saturated and trans fats, as they can raise cholesterol levels and increase the risk of heart disease. Additionally, watch your sodium intake to keep your blood pressure in check. Incorporate foods rich in omega-3 fatty acids, like fatty fish, flaxseeds, and walnuts, as they have been shown to reduce the risk of heart disease. 2. Maintain a Healthy Weight Excess weight can strain your heart and increase your risk of heart disease. Calculate your body mass index (BMI) to determine whether you are within a healthy weight range for your height. If you’re overweight or obese, making gradual changes to your diet and increasing physical activity can help you shed pounds and reduce the strain on your heart. 3. Stay Active Regular physical activity is essential for keeping your heart healthy. Aim for at least 150 minutes... 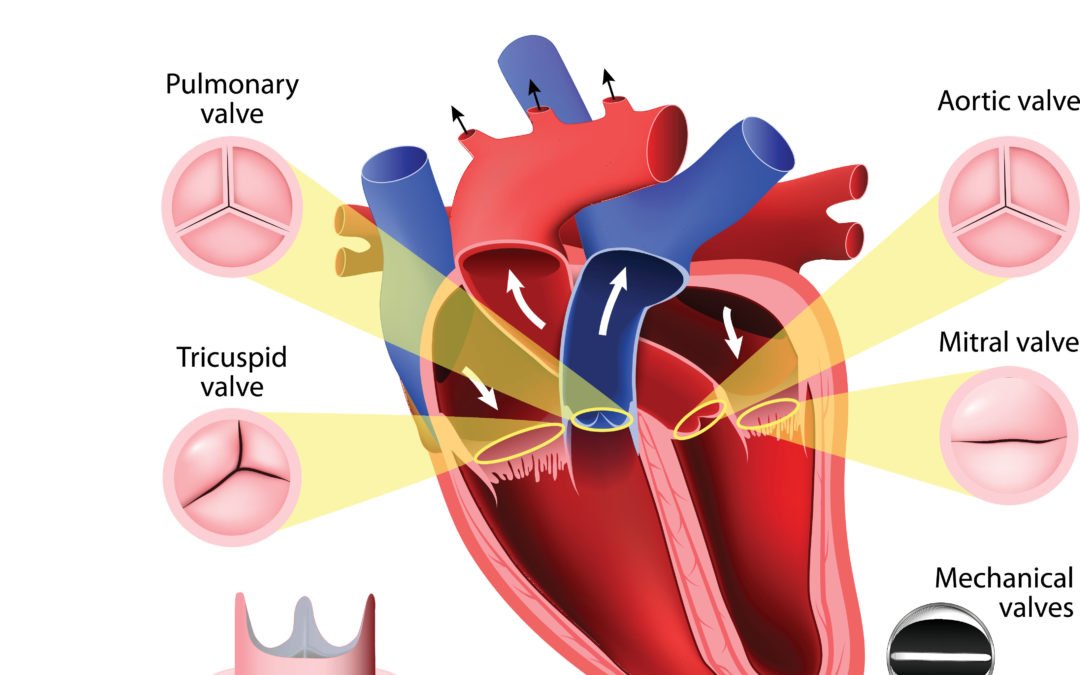
by DrCiuffo | Jan 4, 2023 | Blog, Anatomy
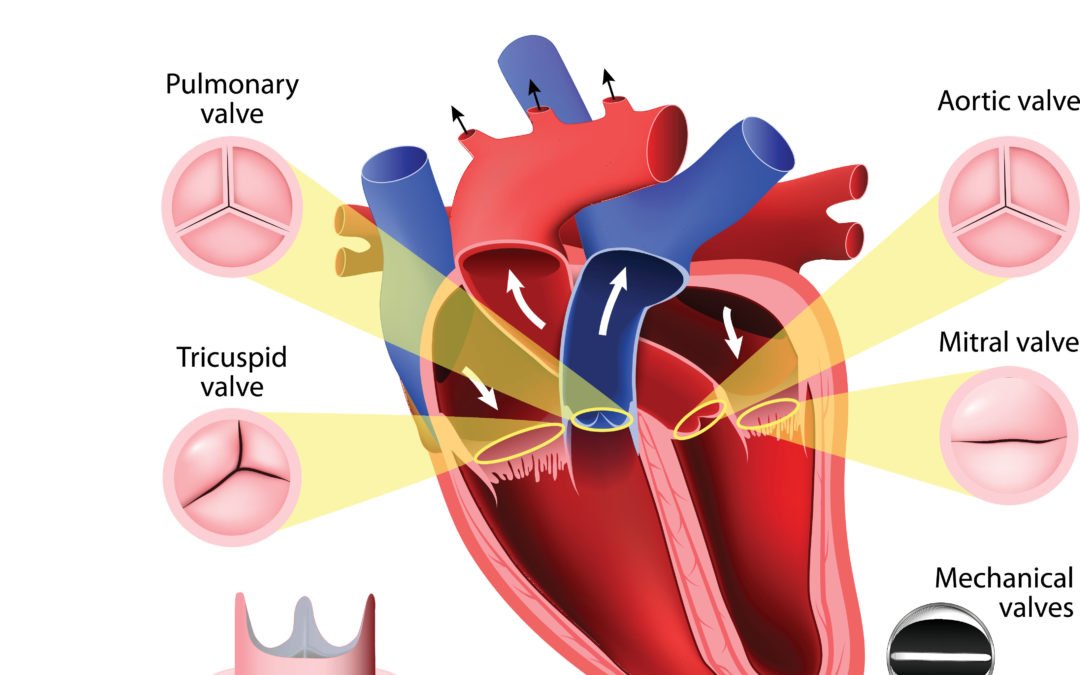
The heart is the symbol of love, affection, and intimacy for many. However, not everyone knows much about the actual the heart’s structure. What is the difference between a valve and a chamber? What are the major arteries and veins? If you don’t know the answers to these questions, then this is blog is going to answer all of your questions about the heart’s structure. Heart Chambers The heart’s structure is divided into four main parts called chambers. These four chambers are divided into two groups: The Atriums are located within the upper part of the heart. There is one is on the right side, and the other is on the left side. Oxygenated blood is pumped through the left atrium into the body. Once the blood has deposited oxygen to other parts of the body, it is pumped into the right atrium of the heart, where it is recycled. The Ventricles are on the bottom of the heart and are often considered its main chambers, which collect blood from the left atrium and expel it toward the lungs. Heart Valves Blood flows through the heart’s structure in one direction from one chamber to the next through a series of valves. These valves consist of tissue that is about as thick as a piece of paper. Like the heart chambers, there are four heart valves between each of the chambers. The tricuspid valve is the right atrioventricular valve. The bicuspid or mitral valve is the left atrioventricular valve is. The pulmonary semilunar valve is between the right ventricle and the pulmonary trunk. The aortic semilunar valve is between the... by DrCiuffo | Dec 30, 2022 | Advanced Heart Surgery, Aortic Valve Replacement, Blog, Dr. Giovanni B Ciuffo, Heart Health
A normal functioning aortic valve has three leaflets, usually referred to as cusps, and is positioned at the end of the left ventricle. This valve is the main pump that delivers oxygenated blood to the entire body. An aortic valve replacement is required if someone suffers from Aortic Valve Stenosis or Aortic Valve Insufficiency. These two issues can cause a significant number of problems and can be life-threatening. Understanding the components that are involved in an aortic valve replacement is essential, especially if you are considering one. Dr. Ciuffo takes the time to consider your specific situation before moving forward on a treatment plan. If you are looking for this information to guide you through decisions regarding your healthy heart, this is a great place to start. Today we take a deep dive into aortic valve replacement, so you can have the knowledge you need. When to Consider Aortic Valve Replacement As already mentioned, there are two reasons why someone would need an aortic valve replacement. When suffering from aortic stenosis, the valve is narrow, causing it to be more challenging for the blood to go through. Basically, the muscle in the heart begins to thicken, causing a hissing sound, which is oftentimes confused with a murmur. With aortic valve insufficiency, the valve tends to “leak” when it is closed. This makes the heart work twice as hard to make the blood flow correctly and in the right direction. To repair this, doctors have created a minimally invasive technique that is much safer and easier on patients. What to Consider for an Aortic Valve Replacement Since the breastbone is...